Tissue Engineering for a Future without Organ Shortages
Q&A with Dr. Roland Gilbert G. Remenyi, Head of Biomedical Research Unit of TMC’s Clinical and Translational Research Institute, on the Tissue Engineering program at The Medical City
What inspired the creation of the Tissue Engineering program at TMC?
The prospect of addressing the critical organ shortage through laboratory-grown tissues is incredibly compelling. Imagine a world where anyone who needs an organ replacement would have the option of receiving one through the power of tissue engineering, rather than having to wait for a donated organ to become available.
At its core, tissue engineering aims to create functional tissues. These can hopefully one day be used to restore and repair damaged tissues of patients here in the Philippines. While challenges remain before we can safely transplant engineered organs, the pursuit of this goal is undeniably inspiring.
How has the program evolved since its inception?
While the creation of fully functional, transplantable organs remains many years away, current tissue engineering technologies offer significant potential. Although we cannot yet replicate complex organs like the heart or liver, we can produce smaller, simplified versions known as “mini-organs.” These miniature models play a vital role in understanding certain diseases, testing the potential of new drug candidates, and studying various pathogens such as viruses and bacteria in a safe laboratory setting.
In phase 1 of our tissue engineering project, we have decided to focus on creating a few tissue models specifically for these purposes, falling under the category of “pre-clinical” research.
What are the most significant achievements of the program to date?
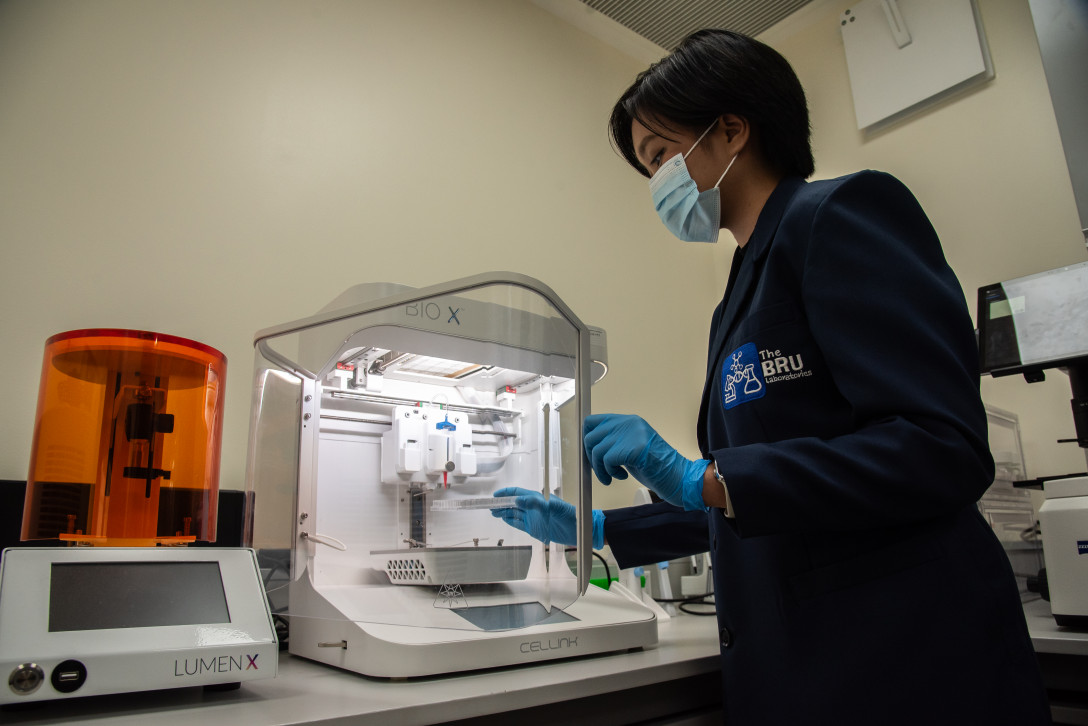
In 2022, our program secured funding from the Department of Science and Technology (DOST) to implement two projects related to tissue engineering. One of these projects involved a collaboration with the University of Santo Tomas and provided a direct link between TMC and an academic laboratory. In 2024, we also received funding for an additional project as part of a collaboration with a local industry partner, Herbanext Laboratories.
We consider it an achievement that TMC is being recognized by the Philippine Council for Health and Development as a private partner that can be trusted with multi-million-peso projects to drive research and innovation in biomedical research. Thanks to this funding, we have been able to provide the training ground for nine young scientists who now boast real-life experience working in a tissue culture lab and have experience with tissue engineering approaches. We are confident that these talented individuals will be at the forefront of the Philippines’ biomedical advancements.
Additionally, our team presented a conference paper at the 2023 International Symposium by the Philippine Society for Cell Biology; their poster presentation highlighted our scoping review of the clinical trial landscape in 3D bioprinting. We have also prepared a manuscript on this scoping review that will soon be submitted to international journals for publication
How do you measure the program’s success and impact on patient care?
One measure of success is whether we have provided a viable solution to an existing problem. I hope that one day, doctors will tell us that the solutions we developed through tissue engineering had helped them in their practice, given their patients hope when previously there was none, or reduced the number of patients requiring toxic treatments. Additionally, we hope that our laboratory findings can be shared with the international community through peer-reviewed research articles and conference presentations, even before we have developed a product that can be used in patient care.
How has the program contributed to the hospital’s overall reputation and standing in the medical community?
I am thrilled that several of our former team members have chosen to further their education. Some have been accepted into PhD programs in the U.S., an MD program in Singapore, a master’s program in Australia, or have decided to pursue medicine here in the Philippines.
As international and local selection committees review their impressive CVs and interview our former lab members, it may be the first time the reviewers have encountered the name “The Medical City”. I hope that our former employees will now serve as ambassadors for TMC, enhancing the hospital’s reputation and attracting new patients.
CHALLENGES AND FUTURE DIRECTIONS
What are the primary challenges facing the tissue engineering program?
Our research is significantly affected by the need to purchase and import materials from other countries. Delays in receiving essential supplies and reagents, such as cell culture reagents, bioinks, and well-characterized cellular materials, can be both costly and time-consuming. A lack of local suppliers in these critical areas further exacerbates these challenges, not only slowing down our progress but also increasing our expenses. Additionally, equipment breakdowns and failures often require specialized expertise that is not readily available domestically, leading to extended downtime. A recent incident involving our bioprinter highlights this issue, as a pump failure necessitated bringing in a foreign expert for repairs.
How do you address the gap between research and clinical application?
We are fortunate to have our research laboratory located within a hospital, allowing us to work closely with clinicians and patients. Sharing our research findings with them early on enables us to receive valuable feedback on the relevance of our solutions for doctors and their patients.
Programs like the Physician Scientist Fellowship bridge the gap between research and clinical practice. Our program offers thematic areas such as tissue engineering, and I am optimistic that future batches of Physician Scientist Fellows will continue to push the boundaries of what is possible with advanced technologies like 3D printing, bioprinting, and tissue engineering. I am confident that future fellows will continue to make groundbreaking strides in this field.
What are the future directions for the program, and how do you plan to achieve these goals?
We intend to make these tissue engineering technologies available to government, industry, and academic partners through service and research collaborations. Our goal is to share these technologies with other institutions; a goal that will be facilitated by the TMC Ventures Office.
For instance, a robust model to confirm antiviral effects against dengue could benefit partners who are developing new anti-dengue drugs. Bioprinted skin models can also be useful for local microbiology labs that are interested in treating antibiotic-resistant bacteria affecting the skin. These new partnerships will help us bring new products to the market faster, benefiting patients sooner.
To achieve these goals, we also anticipate continued support from the DOST. This year, we received a grant from the DOST’s Collaborative Research and Development to Leverage the Philippine Economy (CRADLE), allowing us to collaborate with a local biotechnology company, Herbanext Laboratories, to study the antiviral effects of Tawa-Tawa using our tissue engineering models.
Tawa-tawa (Euphorbia hirta L.), is a herb renowned for its anti-dengue properties, which are attributed to its rich concentration of bioactive compounds.
How do you envision the role of tissue engineering in healthcare in the next 5-10 years?
Our bioprinting team recently completed a review to assess the landscape of clinical trials using 3D bioprinting.
One promising approach is the creation of personalized, patient-specific tumor models that can be tested in the lab. By testing different cancer drugs on these models, doctors can identify the most effective treatment for each patient. This approach has the potential to become a standard part of cancer patient care.
Rather than subjecting the patient’s body to a toxic drug cocktail without certainty of how the cancer will respond, we can “pre-test” a representative model of the patient’s tumor that has been regenerated with tissue engineering approaches in the lab. Once the best medicine combination has been found, patients can be cured more quickly and with fewer side effects.
Tissue engineering has broad applications, including treating burn victims, diabetic foot ulcers, and repairing cartilage and bone. Beyond medicine, it shows promise in creating sustainable food sources, like lab-grown or 3D-printed meat tailored to individual needs and health conditions.
Finally, I hope that we will no longer need animal testing during the drug development process—3D bioprinted tissues could become the gold standard to study the absorption, distribution, metabolism, excretion, and toxicity of new drugs, simulating how the body responds to medication.
TEAM AND RESOURCES
What is the composition of your team, and what are their respective roles?
Thanks to funding from the DOST, each tissue engineering project can hire two team members whose salaries are fully covered by the DOST. These members hold the official job titles of “Project Technical Specialist” and “Project Technical Assistant,” following DOST’s grants-in-aid (GIA) personnel titles. Under this arrangement, team members work together to ensure the effective implementation of each tissue engineering project according to the defined deliverables in the project proposal.
Co-investigators from TMC and partner institutions contribute to the program by offering scientific guidance and expertise in regular progress meetings. Within the tissue engineering team, it’s important for everyone to be supportive and willing to assist each other to ensure that everyone can achieve their project goals.
What kind of support do you receive from the hospital administration?
As our work and projects have expanded, we have seen the need for more space for testing and analysis. An initial funding has transformed an underutilized space on the hospital’s lower ground level into a state-of-the-art research laboratory, which has now become our primary workspace. As scientists, this research facility enables us to make significant contributions to advancements in our field without having to travel abroad.
There is likewise an ongoing support of the annual intramural grant funding, which provides financial support for research studies in biomedical innovations.
Additionally, TMC’s REWARD program, which offers travel and fee assistance for local and international conferences, has been invaluable in facilitating our participation in conferences and sharing our research findings.
How do you attract and retain top talent in tissue engineering?
We typically announce our DOST-funded project vacancies on LinkedIn and Facebook groups related to research in Molecular Biology and Cell Biology. Additionally, I seek recommendations from colleagues, particularly if they are aware of students with prior experience in tissue engineering. Subsequently, we invite potential candidates to our facility for a lab tour, research presentation, and interviews to assess their alignment with the project and their career aspirations in a research scientist role.
COLLABORATION AND PARTNERSHIPS
How does the program collaborate with other departments within the hospital?
We collaborate closely with the Regenerative Medicine Laboratory of the Institute of Personalized Medicine, sharing resources such as an automated cell counter and a fluorescent microscope.
Additionally, we utilize the exceptional diagnostic services of our Department of Laboratory Medicine. For example, we send samples to pathology for processing using routine methods such as H&E stain to demonstrate the successful recreation of skin-like tissue. Our ultimate goal is to create tissue that is indistinguishable from natural human tissue, as verified by expert pathologists.
Similarly, our bioprinted mini livers are evaluated by pathologists to determine if they accurately represent healthy, fatty, or cancerous liver tissue, etc. Our goal is to further collaborate with other departments, such as cosmetic surgery, to explore the potential of tissue-engineered skin for their patients.
What partnerships exist with external institutions or industries?
We would like to express our gratitude to the DOST for their support of our research program through grants-in-aid (GIA) funding. Its Virology and Vaccine Research Development program is backing two of our projects.
One of these projects involves a collaboration between TMC and the University of Santo Tomas. At UST, bacteriophage researchers are using bioprinted skin tissues produced by TMC as infection models for pathogens such as Streptococcus aureus.
Additionally, we are partnering with Herbanext Laboratories, a biotechnology company from Negros Occidental, to study the antiviral effects of Tawa-Tawa using our dengue infection model.
Furthermore, we have close working relationships with local technology suppliers like Rainphil Inc., Merck, CIM Technologies, Noveaulab, DKSH, and ZEISS to stay updated on the latest equipment developments. These partners have helped us organize workshops and demo sessions for new equipment.
We are also excited to collaborate with a local start-up company, Biomats Philippines, to make bioprinting technology more accessible to Filipino labs. For example, Biomats allowed our lab staff to demo a prototype of their proprietary bioprinter.
How important is collaboration in advancing tissue engineering research and development?
Tissue engineering is a highly interdisciplinary field that requires collaboration among team members with diverse skill sets. Chemists, biologists, pathologists, biomedical engineers, microbiologists, and physicians must work together to develop platforms and products that are meaningful and useful to the local community.
In addition, maintaining a sterile environment in a tissue culture facility requires collaboration among all staff members. Any experiments involving biohazardous agents, such as viruses, need to be conducted with proper safety protocols to ensure the safety of all staff members.
ETHICAL CONSIDERATIONS AND PUBLIC PERCEPTION
How does the program address ethical concerns related to tissue engineering and regenerative medicine?
All of our research protocols are registered with TMC’s Institutional Review Board (IRB) to guarantee that we maintain the highest ethical standards. Without approval from our IRB, we cannot move forward with our research study. By considering our IRB as our partner, we ensure that any ethical concerns are identified during the planning stage and addressed before the research is carried out.
What role does patient consent and education play in the program?
One of the challenges in the Philippines is the lack of available cellular materials that accurately represent the genetic makeup of Filipinos. Currently, researchers mainly rely on established cell lines or primary cells that have been developed by experts from other countries, which may not fully reflect the unique genetic background of Filipino patients. Our aim is to create research platforms and pathways that will enable us to ethically and safely study donated cells from Filipino individuals.
In future programs, it will be crucial to communicate to each patient the significant role that donations such as umbilical cords, liver biopsies, tumor biopsies, foreskin, or excess skin from plastic surgeries could play in establishing better research models for studying diseases.
Additionally, we are committed to obtaining informed consent from every patient from whom cellular material is obtained. Recently, our research team watched the movie “The Immortal Life of Henrietta Lacks,” which is based on the true story of Henrietta Lacks as detailed in Rebecca Skloot’s bestselling book. The movie highlights how in 1951, researchers took cells from Henrietta Lacks without her knowledge and used them to create the first “immortal” cell line (the HeLa cell line) that could be perpetually grown in the laboratory. This story serves as a cautionary tale, emphasizing the importance of following proper informed consent practices, anonymization of biospecimens, de-identification, and IRB (reviews to prevent injustices.
How do you communicate the benefits and potential risks of tissue engineering to the public?
Public forums are an excellent way to educate and build trust with the public. The Medical City does a great job at this. They host various events such as lay forums, awareness weeks, and special seminars every week, with a different department hosting an event each time. For example, during the 2023 annual research week, we provided a research lecture on the current state of tissue engineering and its potential applications at TMC. We aim to maintain this vital dialogue to establish trust with our patients.
As a manager, I strive to be open to feedback from our employees and understanding of any challenges they may encounter, whether professional or personal. By demonstrating our openness to input and the belief that everyone can achieve their full potential, we can greatly improve the likelihood of retaining employees throughout their contract terms and beyond.